Psssst. I want to let you in on a little secret.
If you’re feeling a little, well, freaked out about all the weird or scary things that might happen during birth, you’re not alone.
I remember spending tons of time researching and reading and attempting to empower myself before going into labor with my son, and still having a major case of the jitters. There were just so many unknowns; I wasn’t sure if I’d ever be ready.
Of course, it didn’t really matter if I was ready, because that baby was gonna come out, one way or another. And if you’re pregnant, so will yours. So today we’re gonna bust some myths and shatter some fears around childbirth.
In no particular order, here are the answers to those questions you’ve just been too afraid (or embarrassed) to ask.
Fear #1: Pooping in the Delivery Room
That’s right, I said it. And yes—horror of horrors—some women poop while giving birth, right there in the birthing tub or on the hospital gurney. And while that probably ranks way up there on your list of “most embarrassing things that could ever happen, ever,” it really shouldn’t be all that surprising.
The same muscles used to push out a baby, after all, are involved in emptying your bowels.
Back in the day, women were routinely given enemas in the earliest stage of labor to prevent this from happening, but the practice has largely fallen out of favor. Why?
Enemas Debunked
Because it turns out that enemas provide exactly zero benefits to women in childbirth. Despite earlier reasoning, they:
- do not reduce the length of labor (as was previously thought),
- do not lower the risk of infection (from fecal matter contamination, that is—they may actually increase the risk, due to, ahem, anal leakage),
- can be really uncomfortable.
An enema is probably the last thing you’d want at 40 weeks, in fact.
So What’s a Mama to do About the Doo Doo…
First, know that while pooping during delivery is totally possible, it probably won’t happen. The prostaglandins your body releases to help the cervix efface and the uterus contract also have a cramping effect on the bowels. (In the twenty-four hours before I went into labor with my son, I must have gone to the bathroom no fewer than twelve times—by the time I was ready to push, my bowels were pretty much empty.)
But if you do end up doing the ‘doo, you probably won’t even realize it. Nurses and midwives have plenty of experience quickly and discretely cleaning up any accidents, so as not to distract you from the real work at hand. Seriously, these ladies have seen everything—they just wipe it up and keep it moving.
I can tell you, too, that once you’re in active labor, you won’t give a poop about anything other than getting your baby out.
Whatever you do, don’t hold back during the pushing phase out of fear that you’ll poop in the delivery room. You’ll risk lengthening your labor, increasing the pain, and upping your need for interventions.
Fear #2: What If We Don’t Make It to the Birth Center in Time?
Every woman who’s not planning a home birth has thought about it: What if I end up giving birth in the parking lot? Or worse—in the car?!
The thought certainly crossed my mind, and the second time around my fears were almost realized: As we were driving to the birth center on the day of my daughter’s birth, I very nearly instructed my husband to pull over so I could deliver our little bundle right there in the Volkswagen. Fortunately, we arrived just in time—I was “complete and +2” in case you’re wondering—and very nearly delivered my baby on the gurney.
Despite these totally normal, entirely understandable fears, it is extremely rare that a first-timer will wait too long to head to the hospital. In fact, it’s much more likely that you’ll arrive too early.
Still, if you want to get educated, here are step by step instructions on how to give birth in a car, written by a registered nurse on our team. The post includes interviews with mamas who gave birth in cars, plus several car birth videos.

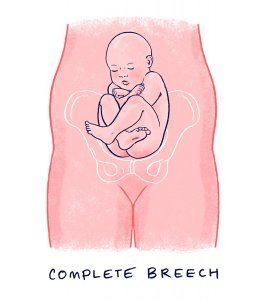
Fear #3: What If My Baby Is Breech?
So you’ve tried moxibustion acupuncture and visited a Webster-certified chiropractor. You’ve had an external cephalic version. You’ve spent the last nine months balancing atop a birthing ball. But now your due date is merely days away, and your baby is still positioned butt-first. What to do?
 Well, you’ve got a few options.
Well, you’ve got a few options.
Option A is to accept the situation for what it is, grieve if necessary, and deliver via gentle Cesarean.
Option B is to find a provider who’s got some experience attending vaginal breech births. Breech is really just another variation of normal and delivering babies in this position has become a lost art.
Katie is very well versed on this topic and you can learn more about her:
- Breech water birth
- and her breech VBAC
According to the American Pregnancy Association, you should meet the following criteria in order to safely attempt a vaginal breech delivery:
- You’re at least 37 weeks along.
- Baby is in the frank breech presentation. (Some providers may green-light a complete breech baby for a vaginal delivery, too, as this is the next most favorable position.)
- Baby shows no signs of distress when his heart rate is closely monitored.
- Baby is not too big to pass safely through the birth canal. (Generally speaking, baby should be no bigger than 4,000 grams, or 8 pounds, 13 ounces.)
- Anesthesia is readily available and a Cesarean delivery possible on short notice.
- Labor is spontaneous and progresses steadily.
If you choose to move forward with a vaginal delivery attempt, know that your odds will improve significantly if you’ve got a skilled provider who takes a “hands-off” approach. Mamas who’ve had one previous vaginal delivery may have a higher chance of success than first-timers.
Fear #4: What If I Have “Back Labor”?
Ouch! So, what exactly is back labor? Well, it’s pretty much self-explanatory: it’s when the full force of labor seems to concentrate in the lower back, directly above the sacrum.
According to the American Pregnancy Association, it’s often accompanied by:
- Irregular contractions
- A labor that’s slow to progress, and
- A prolonged pushing stage.
In other words, exactly like my first childbirth!
The most common cause of back labor is the position of the baby. More specifically, the “occiput posterior” position causes the hardest part of baby’s skull to put pressure squarely on mama’s tailbone.
I’m not going to lie to you: this does not feel good. It’s not unbearable, it’s just really, really uncomfortable.
Managing Back Labor
So how do you fix it?
First things first. If you think you’re experiencing back labor, get up and get moving. Lying on your back only encourages baby’s full weight to rest on your spine. (If you must lie down, try lying on your side.)
To encourage baby to move into a more favorable position, try:
- Walking around
- Squatting
- Lunging, or
- Dropping down onto your hands and knees and doing some pelvic rocks
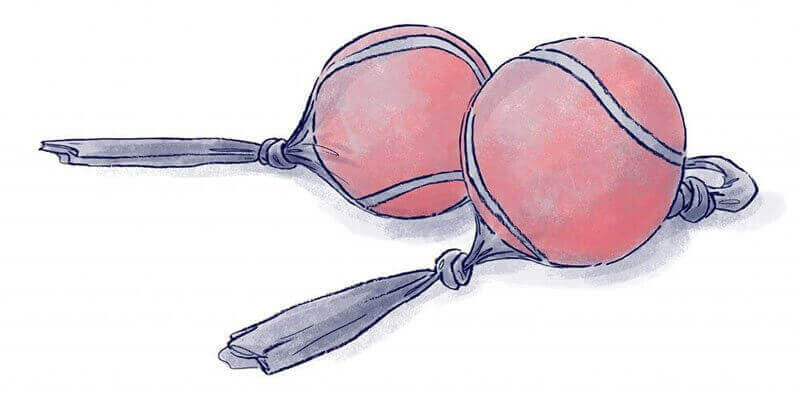
As for pain relief, counter pressure works wonders. Have your partner, doula, or labor support person use a ball type massager or apply pressure to the points located on either side of your spine. Or try leaning forward in the shower and directing the flow of hot water directly onto your back.
You can also soothe your back muscles by using a heated rice sock. (Basically, this is just a DIY hot water bottle: pour some uncooked rice into a tube sock, tie a knot at the top, and heat to the desired temperature in a microwave.)
Fear #5: What If My Labor Stalls?
A lot of “stalled labor” has to do with the outdated guidelines used to determine how quickly a “normal” labor should proceed.
Thankfully, the American College of Obstetricians and Gynecologists released new guidelines in 2014, redefining the start of active labor as dilation to 6 centimeters (rather than 4) and urging doctors to allow women to labor longer, so long as the baby is not in distress.
According to the new standards, first-time mamas should also be allowed to push for at least three hours, longer if they’ve had an epidural. These changes, however, take time to implement. Your doctor may still adhere to the old standards.
How Can You Lessen Your Chance for an Unnecessary Cesarean?
First, remember that it’s imperative to stay home as long as is safely possible. (This is where doulas can be such a help!)
The less time you spend on the hospital’s clock, the less you’ll be pressured to give birth within some arbitrary time frame.
Once you are admitted, you’ll want to create as calming and relaxing an environment as possible…
- Turn the lights down
- Listen to soothing music
- Diffuse your favorite essential oil
- Practice your childbirth affirmations
- Drown out the distractions around you
All these activities can help create a sense of safety, which can reduce your output of labor-stalling stress hormones.
If at some point, your labor does stop progressing, turn to natural remedies to augment your contractions, nipple stimulation and homeopathic remedies are a good place to start.
Fear #6: What If My Vagina Tears?!
I’m not sure if there’s anything that sounds worse than having a “tear” in your vagina— it just makes your skin crawl, doesn’t it?
But there’s no getting around it: during birth, the vagina and the perineum (the area between the vagina and anus) have to s-t-r-e-t-c-h, and sometimes that delicate skin just can’t stretch quite fast enough.
Anywhere from 40 percent to 85 percent of women delivering vaginally will experience some level of tearing, according to the American College of Nurse-Midwives.
However, the severity of the tear can vary widely. In fact, there are four distinct types:
- First degree: A first-degree tear is the least severe, involving only the skin, and will require minimal stitches to repair, if any. It should heal completely within a week or two.
- Second degree: Second-degree tears are a little more serious, in that they involve the skin and the muscle underneath the skin. They typically require a few stitches to close, and heal within two to three weeks.
- Third degree: A third-degree tear involves the skin, the perineal muscle, and the muscle that surrounds the anus (the anal sphincter).
- Fourth degree: By far the most serious, fourth-degree tears include the skin, the perineal muscle, the anal sphincter, and the tissue that lines the rectum.
Here’s the Good News
Third- or fourth-degree tears are uncommon, occurring in just 2 to 4 percent of vaginal births.
Want to Lower Your Risk of Tearing?
I wish I could give you a foolproof solution (with a 100 percent money-back guarantee)—but there isn’t one.
But, Perineal massage can help, as can opting for a natural childbirth (Pitocin and epidurals are both associated with a higher risk of tears).
But Let me Get Real With You
Tearing was my second biggest fear walking into my first birth, right behind having a C-section. And guess what? I ended up with a second-degree laceration.
I didn’t feel it one bit, and it healed up in a snap. In fact, my midwife explained her love and appreciation for the bounce-back-ability of the vagina like this: “Slap it together, put some stitches in it, and it’s good as new.”
Yes, she really did say that.
And, yes, I found her words to be true.

Want to Help Change the Birth Culture in our Country?
It starts by getting informed. I’ve just published the first week-by-week pregnancy guide from a natural perspective. Featuring insights from a certified nurse midwife (who happened to deliver both of my children), as well as a registered nurse and doula, the book is packed with helpful info on:
 Natural remedies for common pregnancy symptoms
Natural remedies for common pregnancy symptoms- When to get an ultrasound (and when not to)
- Sex during pregnancy
- The truth about epidurals
- How to naturalize a surgical birth
- Natural pain relief during labor
- What to do during every stage of labor
- How to recover naturally
- And so much more
This book is evidence-based, empowering and entertaining. (No boring text books over here!)
If pregnancy is in your future, or if you know someone who is pregnant, please consider picking up a copy.
Support and Help for Mamas
While some mamas do get the birth of their dreams, I know firsthand that it doesn’t always work out that
way. But if we come from an informed place, we can feel good about the experience no matter what.
I hope every mama out there gets the support and resources she needs to have an empowered and grace-filled birth.
 About Genevieve: Genevieve Howland, aka Mama Natural, has a wonderful free pregnancy week-by-week series from a natural perspective. I loved her pregnancy materials so much that I signed up for her amazing online birth classes with my last pregnancy. Genevieve is helping to change the culture of childbirth in our country and is taking her mission to the next level with a beautiful new book that is out this week, The Mama Natural Week-By-Week Guide to Pregnancy & Childbirth.
About Genevieve: Genevieve Howland, aka Mama Natural, has a wonderful free pregnancy week-by-week series from a natural perspective. I loved her pregnancy materials so much that I signed up for her amazing online birth classes with my last pregnancy. Genevieve is helping to change the culture of childbirth in our country and is taking her mission to the next level with a beautiful new book that is out this week, The Mama Natural Week-By-Week Guide to Pregnancy & Childbirth.What pregnancy or childbirth fears do you have? Is this info helpful? Share below!


Leave a Reply